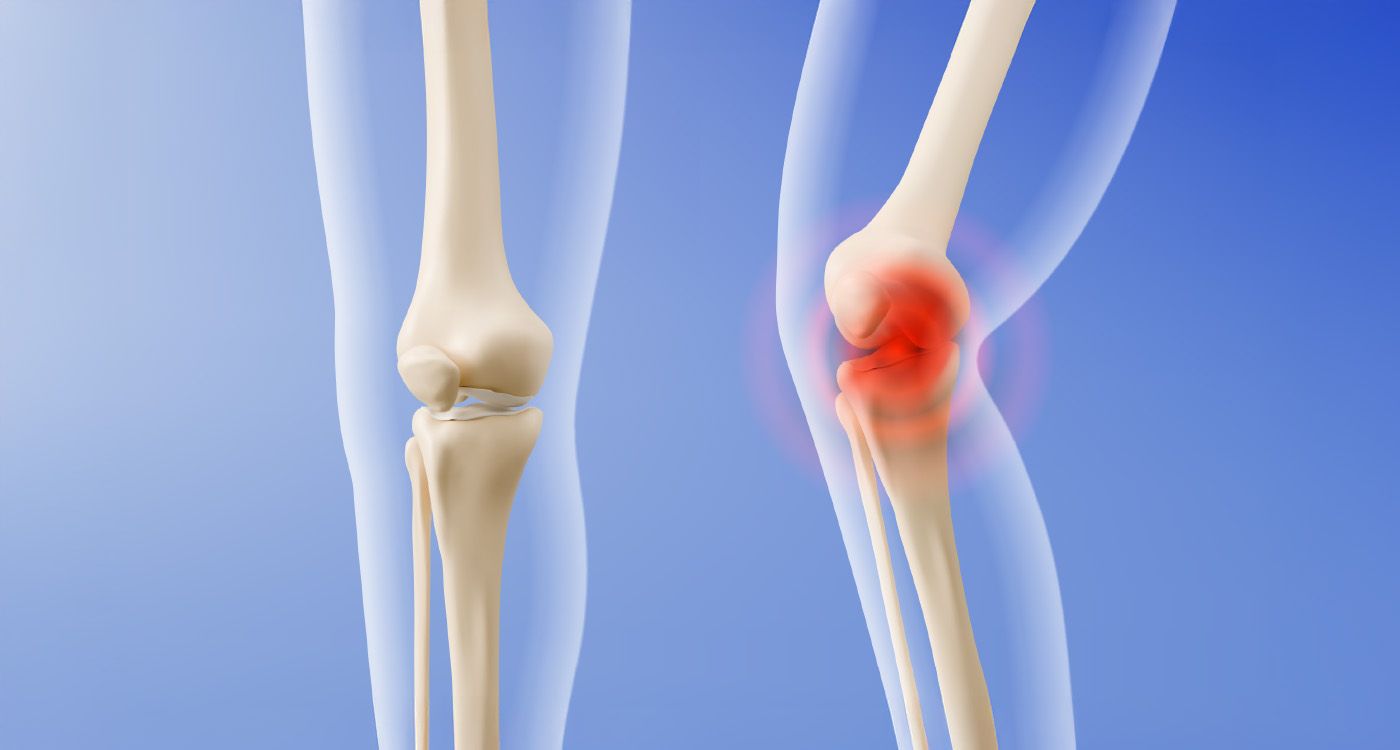
In the ongoing fight against arthritis, where every step is a struggle, a team of researchers from Cambridge offers new hope: an “intelligent” artificial cartilage that releases medication at just the right moment. A biomedical breakthrough or just an illusion?
This morning, in the calm corridors of a hospital, Myriam, 56, hesitates before putting her foot on the ground. Arthritis, with its constant flare-ups and stiffness, waits behind every movement. Around the world, hundreds of millions of people live in fear of a single misstep, caught between brief moments of relief and the anxiety of the next flare-up.
Science now offers a possible solution: an “intelligent” artificial cartilage developed by researchers at the University of Cambridge.
Their goal is to create a targeted treatment that releases anti-inflammatory drugs only when the joint becomes inflamed, reducing the side effects of traditional therapies.
But how much can we trust the promise of personalized medicine? And can such technology be embraced without losing sight of the human dimension it touches?
On October 21, 2025, in the Journal of the American Chemical Society, Professor Oren Scherman’s team revealed the result of five years of research: a polymer hydrogel that is as flexible as natural cartilage but with an extraordinary ability. This material can detect even the slightest change in pH, an early sign of joint inflammation. “We wanted to create a material that’s not just a passive substitute, but an active part of the healing process,” Scherman explained on the University of Cambridge website.
During an arthritic flare-up, the affected joint becomes slightly more acidic. The hydrogel, built with molecular bonds that react to acidity, softens and releases anti-inflammatory drugs directly at the affected site. In the lab, the team has already demonstrated the mechanism: a fluorescent marker trapped in the material is released only when the pH drops, simulating inflammation.
The idea of reducing the need for widespread medication and its side effects now seems tangible. One major hurdle remains. So far, the tests have only been conducted in test tubes and on animal models. Human trials are still a long way off and will face both biological and ethical challenges.
A Technological Gamble
The secret behind this new generation of cartilage lies in the delicate chemistry of hydrogels, inspired by nature but designed to go beyond its limits. These polymer networks are woven with macrocycles (cucurbit[n]uril), molecular gatekeepers that open or close depending on the surrounding acidity. At a normal pH, the hydrogel remains stable; under inflammatory stress, its structure loosens, releasing its medicinal payload. This “intelligent” response, explains Dr. Scherman, “allows for highly targeted delivery and constant adaptation to the patient’s condition.”
On paper, the benefits are clear: fewer risks of overdosing, fewer side effects, and better protection for the joint. But questions remain. Can the material withstand the friction and mechanical wear of a human joint? Will the drug release be precise enough to avoid overreaction or too weak to relieve pain? How will the immune system respond? Will it treat the gel as a helper or as a foreign body? Only large-scale clinical trials can provide answers.
Fears and Hopes
At the family table, the conversation comes alive. Myriam, a mother of two, does not dare to hope too much. She both fears and relies on medication: it brings relief but takes a toll on her stomach and kidneys. For her, and for millions of patients worldwide, the idea of an internal, invisible patch that only reacts when inflammation strikes feels like science fiction.
Even technology meant to help can raise concerns. Some worry it could go too far, with people constantly monitored by intrusive devices. Others see it as a way to give back independence to those whose mobility is fading. Health professionals welcome the innovation but emphasize the need to test its reliability over the long term and in real-life conditions. Patient groups stress that social acceptance will depend on how easy it is to use and how affordable it is. It is also important to remember that the gap between a concept and a working clinical treatment is still significant.


Comments