On World Osteoporosis Day, This is Beirut gets to the essentials: the key reflexes to screen for, prevent and treat a silent disease with heavy consequences after age 50. IOF campaigns, targeted screening, lifestyle measures, calcium and vitamin D tailored to need: the goal is to avoid the first fracture.
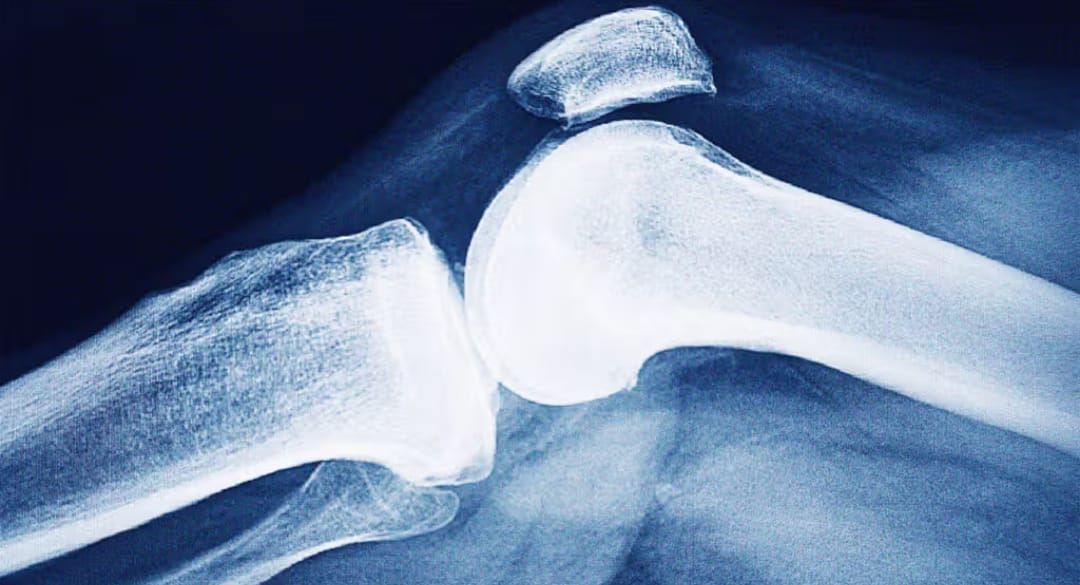
Osteoporosis weakens bone and exposes people to so-called “fragility” fractures (a fall from standing height, a trivial movement). Long asymptomatic, it often declares itself with a first fracture – vertebra, wrist, hip – which is likely to be followed by others if nothing is done. Each October, the International Osteoporosis Foundation (IOF) underscores the scale of the burden and the need for a systematic post-fracture care pathway.
What Is Osteoporosis?
A reduction in bone mass and quality, and therefore in its strength, with an increased fracture risk. Diagnosis relies on bone densitometry (DXA): a T-score ≤ −2.5 at the spine or hip confirms osteoporosis, even without a fracture. “Peak bone mass” is built up into adulthood, remains stable until around age 40, then declines by about 1–2% per year; after menopause, loss accelerates due to estrogen deficiency.
Who Is Most Affected?
Risk increases with age and menopause, but men are also exposed. After a hip fracture, one-year mortality remains high – often higher in men – calling for vigilance.
Screening: who, when, how?
• Women ≥ 65: DXA recommended.
• Postmenopausal women < 65: DXA if risk factors (fragility fracture, prolonged corticosteroid therapy, low BMI, smoking, alcohol, inflammatory diseases, hyperthyroidism, malabsorption, etc.).
• Men: no systematic screening; case-by-case assessment according to risk factors.
Refining Risk: FRAX
To estimate 10-year fracture risk and guide treatment decisions, the FRAX tool (with or without BMD) is widely used in clinical practice.
Prevention: the Non-Negotiable Foundation
Protecting bone means combining a calcium-rich, adequate protein intake; vitamin D tailored to lab status (sensible sun exposure and, if needed, supplementation); and weight-bearing physical activity with balance training to limit falls.
• Diet: aim for 1,000–1,200 mg of calcium per day, prioritizing foods (dairy products, sardines with bones, leafy greens, calcium-rich mineral waters), and ensure sufficient protein intake (meat, fish, eggs or plant alternatives such as legumes, soy, whole grains).
• Vitamin D: measured sun exposure; supplement if deficiency is confirmed or risk factors are present, with usual reference intakes around 800–1,000 IU/day after age 50, to be adjusted based on laboratory results and comorbidities.
• Movement: 20 to 30 minutes of daily weight-bearing activity (brisk walking, stairs, dance), two weekly strength sessions and balance exercises (yoga, tai chi, proprioception) to reduce fall risk.
• Lifestyle: quit smoking, moderate alcohol intake; limit excess salt and coffee (maximum three cups per day), which increase urinary calcium loss; correct vision issues and make the home safer (lighting, rugs, grab bars).
Bone aging is universal, but osteoporosis is not inevitable: prevention and targeted screening genuinely modify risk.
Treatment: A Strategy, not a List
Treatment is based on risk (DXA, FRAX, prior fracture), not “for life” by default. Any initiation of therapy goes hand in hand with correcting deficiencies, physical activity and active fall prevention. After a fracture, a post-fracture pathway (Fracture Liaison Service) markedly reduces recurrence: this is a secondary-prevention priority.
Common Myths: True/False
• Vitamin D alone prevents fractures: false in community-dwelling, non-deficient adults.
• Screening concerns only women: false; in men, assess at-risk profiles and the higher post-hip-fracture mortality.
A Patient’s Voice
Zeina N., 62: “A slip in the kitchen, a wrist fracture. I had never ‘thought’ about my bones. DXA, correction of my vitamin D, start of treatment, two strength sessions per week, safer home. The turning point? Realizing that a first fracture often leads to others if you don’t act quickly.”
Takeaway
After 50, talk to your doctor about screening (earlier if you have risk factors), keep moving and strengthening, make your home safer, and cover your calcium and vitamin D needs according to your tests. The best fracture is the one that never happens.

Comments