A patient living with HIV was declared to be in remission following a bone marrow transplant in 2020, becoming the first such case in France and the eighth globally to be cured of the infection. This case paves the way for a new era in HIV treatment, although this solution remains difficult to apply on a large scale at present.
A patient with acquired immunodeficiency syndrome (AIDS) was declared in remission after undergoing an allogeneic bone marrow transplant in 2020, according to a press release from the Assistance Publique – Hôpitaux de Marseille (AP-HM), published on Friday, January 17. This case represents the first success of its kind in France and the eighth worldwide. The patient, who had been followed since 1999 for HIV, developed acute leukemia a few years ago. As part of her treatment, she received a transplant of hematopoietic stem cells. These cells, responsible for producing the body's three main blood cell lines – red blood cells, white blood cells, and platelets – helped regenerate the patient's blood system and treat her cancer.
Recent tests also confirmed the absence of viral reservoirs, thus indicating her (probable) cure from HIV infection. This new remission, a rare phenomenon, raises hopes for curative treatments for others living with this viral disease. However, this therapeutic perspective remains highly specific and difficult to apply to a broader patient population. So, what explains how this woman was cured of AIDS?
A Generalizable Solution
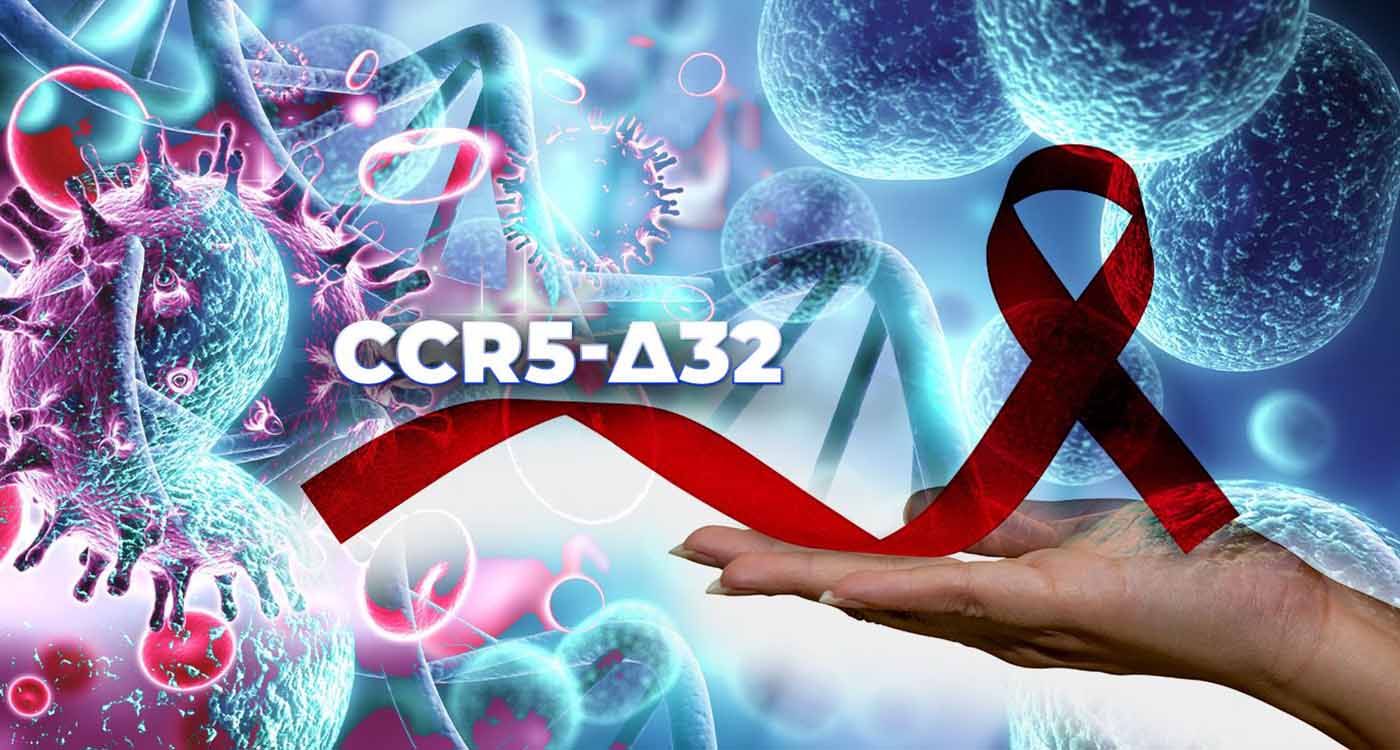
To better understand this scientific victory, it’s important to review the details of the case. After 20 years of effective HIV management with antiretroviral treatment, the patient developed acute myeloid leukemia. Indeed, HIV infection increases the risk of infectious and cancerous complications in immunocompromised individuals. A bone marrow transplant was recommended as the only potentially curative treatment option for her cancer after the failure of other medications. She received an allogeneic transplant from a donor with a well-documented genetic mutation, known as CCR5-Δ32, which prevents HIV from using the CCR5 coreceptor to enter and infect immune cells. According to several studies, this key mechanism may be linked to the cure of HIV infection. After the transplant, the patient continued antiretroviral therapy for three years until ultrasensitive tests showed the complete absence of the virus, suggesting functional remission.
It is important to emphasize once again that this strategy is not a generalizable solution. On the contrary, it represents a major medical challenge, requiring the identification of an immunogenetically compatible donor to prevent rejection. Additionally, since less than 1% of the population carries the protective mutation against HIV, the likelihood of finding a compatible donor with this mutation is extremely low. As a result, performing and succeeding in such a transplant remains a rare and difficult phenomenon to replicate.
A Broader Pool of Donors
Since the first documented cure case in Berlin in 2007 with Timothy Ray Brown, stem cell transplants have generated significant interest as a potential option for eradicating HIV. In most cases, the selected donors carried two copies of the CCR5-Δ32 mutation, one inherited from each parent, making them homozygous. However, the seventh remission case, identified in July 2024, challenged this trend, as the donor carried only one copy of the mutation. According to statistical data from Northern Europe, the likelihood of finding a person with one copy of CCR5-Δ32 is about 16%, compared to 1% for two copies. This case suggests that the pool of potential donors could be expanded, with HIV remission being achievable even with a less pronounced form of natural resistance to the virus. This therapeutic victory adds to previous cases, such as those of Adam Castillejo, a patient from London, and Marc Franke in Düsseldorf, who have all stopped their antiviral treatment without relapse.
Complex Interaction
The emergence of cure cases, including the patient from Marseille, highlights the potential importance of the CCR5-Δ32 mutation. However, researchers believe that several factors are likely involved in the functional remission of HIV. The individual susceptibility of white blood cells (particularly T lymphocytes), the size of the viral reservoir, and the immune response specific to each patient seem to play a crucial role. Thus, the results may not be solely related to the mutation but rather to a complex interaction between the patient's immunological elements and the characteristics of the graft. Further studies are necessary to better understand the remission mechanisms, particularly in cases where the donors did not possess the CCR5-Δ32 mutation.
For example, in February 2022, researchers reported the case of an HIV-positive patient from New York with leukemia who received a combined transplant of cord blood cells carrying the CCR5-Δ32 mutation and adult stem cells without this mutation. Three years later, the patient, who represents the third global case of remission, showed no trace of HIV after stopping antiretroviral treatment. The results were published in March 2023 by Hsu et al. in the journal Cell. This observation is particularly relevant because cord blood stem cell transplants do not require perfect compatibility with the recipient, making them more accessible than bone marrow-derived stem cells.
Genetic Manipulation
These advances revive hopes of a cure for nearly 40 million people living with this disease worldwide, according to the World Health Organization. Scientists agree that multiple factors are likely at play, and a deeper understanding of the underlying mechanisms is essential to apply these findings on a larger scale. However, while the chance of finding a compatible donor with the CCR5-Δ32 mutation remains rare, some researchers have gone further by genetically modifying donor cells to insert this mutation. The “molecular scissors,” known as CRISPR/Cas9, have been successfully used to introduce the modification into stem cells.
A clinical study led by Xu et al., published in September 2019 in The New England Journal of Medicine, reports the case of a patient infected with HIV-1 and diagnosed with acute lymphoblastic leukemia, who received a genetically modified bone marrow transplant using CRISPR/Cas9. The donor cells integrated well, and the patient remained in complete remission from leukemia for 19 months after the transplant, during which the modified cells persisted. No side effects related to the genetic editing were observed.
However, this approach was not sufficiently effective in curing the HIV infection. The coming years will likely be crucial in this regard. Let’s keep our fingers crossed!



Comments